
Quick Links
Resources
About myPHteam
Powered By







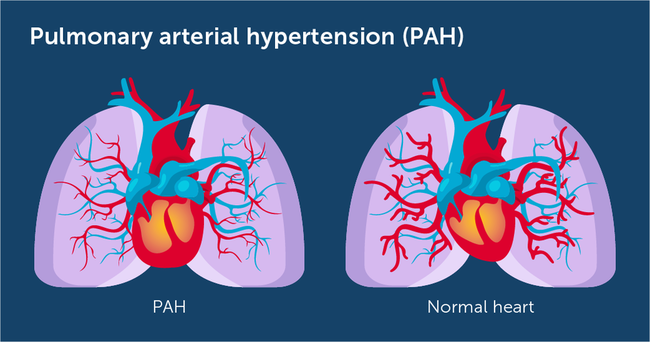
Pulmonary arterial hypertension (PAH) is a rare and progressive disorder that causes tiny blood vessels in the lungs to narrow and create high blood pressure in the lungs. Pressure in the lungs causes the right side of the heart to work harder than normal. Over time, increased blood pressure in the lungs can damage the heart.
 | What Is the Difference Between PH and PAH? |
Pulmonary hypertension is a condition in which the blood pressure is too high in the arteries that carry blood from the heart to the lungs. There are five types of pulmonary hypertension as described by the World Health Organization. PAH is one type of PH. In PAH, high blood pressure in the lungs is specifically caused by narrowed, thickened blood vessels in the lungs.1 Other types of PH have other causes. Right-side heart pressure is usually much higher in people with PAH than in those with other types of PH.2
 | How Does PAH Affect the Body? |
To understand PAH, it helps to know how the heart circulates blood through the body and through the lungs. The heart has two sides - left and right - each of which has pumping chambers (ventricles) and receiving chambers (atria).
The left ventricle pumps blood through arteries to supply oxygen and nutrients to the body. Because blood must travel a long distance from the heart, it needs a lot of pressure. When you get your blood pressure checked, it’s measuring the pressure needed to push oxygenated blood to the body. The blood then returns to the heart through veins on the right side of the heart. The right ventricle doesn’t need a lot of pressure to send blood back through the pulmonary artery to the lungs because the heart and lungs are close together. The pressure required to pump blood from the right ventricle through the lungs is called pulmonary pressure.3
When pumping pressure is too high on the left side, it’s called hypertension or high blood pressure. When it’s too high on the right side of the heart, it’s called pulmonary hypertension.3
With PAH, thickened blood vessels in the lungs can cause high blood pressure in the right heart. The narrowing of blood vessels requires the right side to pump harder to move blood. It also causes a backup of blood returning from the veins to the heart. The right side must work harder to keep up with blood flow. Over time, this can weaken the heart, leading to heart failure. It can also take longer for blood to pick up new oxygen from the lungs. Problems with oxygen circulation can lower the level of oxygen in the blood, creating a risk for brain damage.3
 | What Causes PAH? |
The exact causes of pulmonary arterial hypertension are not always known. PAH may be inherited, caused by another disease or condition, or have no known origin.4 Researchers think that most people who develop PAH have blood vessels that are extra sensitive to internal or external factors that cause narrowing or constriction.5
 Genetics. Approximately 15 to 20 percent of people with PAH have inherited the condition (known as heritable PAH). They may have a mutation on the BMPR2 gene or family history of PAH. While a genetic mutation or family history are risk factors for PAH, they do not guarantee developing it – 80 percent of people with a mutated gene do not develop PAH. A person with a PAH gene mutation has a 50 percent chance of passing that gene along to offspring.5
Genetics. Approximately 15 to 20 percent of people with PAH have inherited the condition (known as heritable PAH). They may have a mutation on the BMPR2 gene or family history of PAH. While a genetic mutation or family history are risk factors for PAH, they do not guarantee developing it – 80 percent of people with a mutated gene do not develop PAH. A person with a PAH gene mutation has a 50 percent chance of passing that gene along to offspring.5
 Medical conditions. When PAH results from medical conditions, it’s known as associated pulmonary arterial hypertension (APAH).5 A number of diseases and conditions can cause narrowing of the tiny blood vessels in the lungs, including those in the chart below.
Medical conditions. When PAH results from medical conditions, it’s known as associated pulmonary arterial hypertension (APAH).5 A number of diseases and conditions can cause narrowing of the tiny blood vessels in the lungs, including those in the chart below.
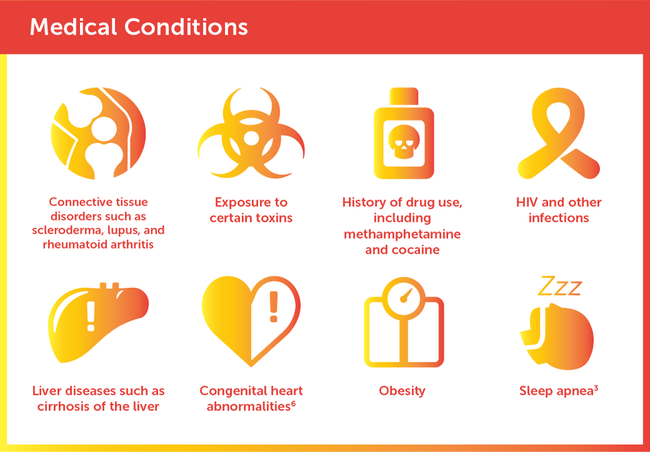
About 30 percent of people with PAH have connective tissue disease.5
 Unknown origin. When no other disease or genetics associated with PAH is present, it is referred to as idiopathic pulmonary arterial hypertension (IPAH).
Unknown origin. When no other disease or genetics associated with PAH is present, it is referred to as idiopathic pulmonary arterial hypertension (IPAH).
 | Risk Factors for PAH |
PAH is three to five times more common in women and typically affects those between the ages of 30 and 60. Women of childbearing age are at greatest risk for PAH.6
A rare form of PH can affect individuals living at high altitudes. For this reason, people with PAH - or even a family history of PAH - are discouraged from living at high altitudes.5
 Early PAH Symptoms
Early PAH Symptoms
There may be no signs or symptoms of PAH in its early stages. Symptoms of PAH can also mimic other conditions.2, 5 PAH may be mistaken for asthma, emphysema, and chronic obstructive pulmonary disease (COPD).3 It’s important to provide your physician with accurate symptoms so they can order the proper tests.2 Let your doctor know if you experience any of the following:
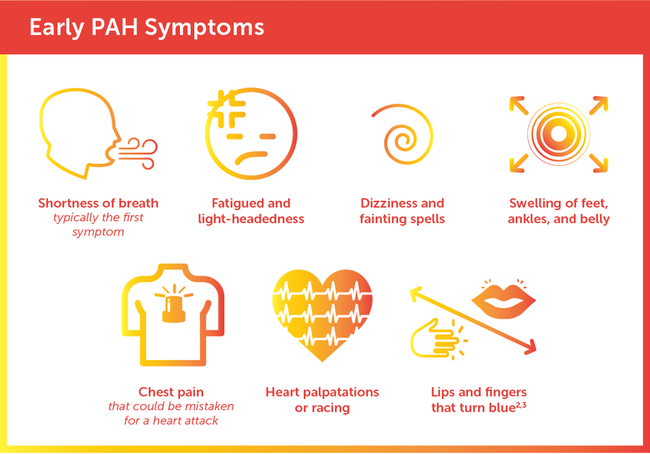
An enlarged heart may be present in people with PAH. Coughing - sometimes with blood - is a rare symptom.5
 | Complexities of Diagnosing and Treating PAH |
Because symptoms of PAH are similar to other diseases that create lack of oxygen in the blood, it can be hard to detect during a routine clinical exam, even if the disease has progressed.5 Early diagnosis and treatment are important to limit the progression of PAH.2
Read more about How PAH Is Diagnosed and Treated.
By sticking to your prescribed treatment plan and making certain lifestyle changes, you can take an active role in managing your PAH symptoms and slowing progression of the disease. Below are steps that can help keep you on track and support your quality of life.
 Stay on your medication schedule: Medication schedules for PAH can be complicated and require close attention each day. It’s important to keep track of supplies and not run out.3 Carry your health information with you at all times and take advantage of smartphone apps that remind you to take your medications.7
Stay on your medication schedule: Medication schedules for PAH can be complicated and require close attention each day. It’s important to keep track of supplies and not run out.3 Carry your health information with you at all times and take advantage of smartphone apps that remind you to take your medications.7
 Schedule follow-up tests and exams: With PAH, follow-ups are initially required every three to four months. You may also receive regular tests, such as echocardiograms and six-minute walk testing. Some doctors will order annual heart catheterizations to see if treatments are helping your PAH and heart function.3 To keep track of your appointments, enlist the help of a family member or friend, or add calendar reminders to your cell phone before you leave the doctor’s office.
Schedule follow-up tests and exams: With PAH, follow-ups are initially required every three to four months. You may also receive regular tests, such as echocardiograms and six-minute walk testing. Some doctors will order annual heart catheterizations to see if treatments are helping your PAH and heart function.3 To keep track of your appointments, enlist the help of a family member or friend, or add calendar reminders to your cell phone before you leave the doctor’s office.
 Avoid stimulants: Stopping smoking can help reduce the strain on the heart and lungs and make a big difference in your symptoms and overall condition.8 Eliminating other stimulants such as cocaine or methamphetamine is also important in managing blood pressure in the heart.3 If you take medically prescribed stimulants for another diagnosed condition, discuss the risks and benefits of these medications with your doctor.
Avoid stimulants: Stopping smoking can help reduce the strain on the heart and lungs and make a big difference in your symptoms and overall condition.8 Eliminating other stimulants such as cocaine or methamphetamine is also important in managing blood pressure in the heart.3 If you take medically prescribed stimulants for another diagnosed condition, discuss the risks and benefits of these medications with your doctor.
 Manage your weight: Excess weight can add pressure on the heart and lungs. Talk to your doctor about the right nutrition and weight for you. Keeping track of your weight is a good way to monitor fluid retention. If weight goes up, your doctor may change your medications.3
Manage your weight: Excess weight can add pressure on the heart and lungs. Talk to your doctor about the right nutrition and weight for you. Keeping track of your weight is a good way to monitor fluid retention. If weight goes up, your doctor may change your medications.3
 Adopt a low-salt diet: Since PAH can lead to a form of heart failure, a low-salt diet with limited fluid intake is important. Salt is hidden in many processed foods and can create fluid retention and swelling. It’s also important to make dietary changes that support your treatment plan, and follow a nutritious diet that’s low on meat and fat and high in fresh fruits, vegetables, and grains.3
Adopt a low-salt diet: Since PAH can lead to a form of heart failure, a low-salt diet with limited fluid intake is important. Salt is hidden in many processed foods and can create fluid retention and swelling. It’s also important to make dietary changes that support your treatment plan, and follow a nutritious diet that’s low on meat and fat and high in fresh fruits, vegetables, and grains.3
 Exercise carefully: It may be challenging, but exercise is important for slowing disease progression and keeping your body strong. A supervised cardiac and pulmonary rehabilitation program that specializes in PAH can help you find the right exercises for your capabilities. Licensed therapists will demonstrate how to safely move your body and build strength, while conserving energy to avoid fatigue and shortness of breath.3
Exercise carefully: It may be challenging, but exercise is important for slowing disease progression and keeping your body strong. A supervised cardiac and pulmonary rehabilitation program that specializes in PAH can help you find the right exercises for your capabilities. Licensed therapists will demonstrate how to safely move your body and build strength, while conserving energy to avoid fatigue and shortness of breath.3
 Stay up to date on immunizations: Get your pneumonia and annual flu vaccines to avoid illness and complications.3 The flu virus can cause inflammation that may worsen PAH.9 It’s also important to reduce your risk of developing pneumonia, which is the cause of death in 7 percent of people with PAH as well as the leading cause of death in people with compromised heart and lung functioning in general.10
Stay up to date on immunizations: Get your pneumonia and annual flu vaccines to avoid illness and complications.3 The flu virus can cause inflammation that may worsen PAH.9 It’s also important to reduce your risk of developing pneumonia, which is the cause of death in 7 percent of people with PAH as well as the leading cause of death in people with compromised heart and lung functioning in general.10
 Pregnancy: Pregnancy with PAH presents challenges and may cause health risks for you and your baby. Talk to your doctor about whether pregnancy is safe for you.6
Pregnancy: Pregnancy with PAH presents challenges and may cause health risks for you and your baby. Talk to your doctor about whether pregnancy is safe for you.6
 Depression and anxiety: Many people with PAH may feel depressed or anxious. It also can be hard to maintain personal relationships and regular levels of activity when you’re not feeling well. Medication, talk therapy, and support groups can help you and your family.3
Depression and anxiety: Many people with PAH may feel depressed or anxious. It also can be hard to maintain personal relationships and regular levels of activity when you’re not feeling well. Medication, talk therapy, and support groups can help you and your family.3
 Travel: It can be challenging to travel with PAH. Talk to your doctor about any supplies, medication, or extra oxygen you may need while traveling. You may also want to identify resources for accessing medicine, oxygen, or health care during your trip, so you’re prepared in case of emergency.3
Travel: It can be challenging to travel with PAH. Talk to your doctor about any supplies, medication, or extra oxygen you may need while traveling. You may also want to identify resources for accessing medicine, oxygen, or health care during your trip, so you’re prepared in case of emergency.3
 Finding support: Several organizations and programs help people with PAH as well as their family members and caregivers. The Pulmonary Hypertension Association helps people with PAH find medical specialists and facilities with expertise in PAH and provides access to in-person support groups.3
Finding support: Several organizations and programs help people with PAH as well as their family members and caregivers. The Pulmonary Hypertension Association helps people with PAH find medical specialists and facilities with expertise in PAH and provides access to in-person support groups.3
How Long Does It Take For The Combination Of Tadalafil And Ambrisentan Before It Reduces Shortness Of Breath?
Sign up for free!
Become a member to get even more




A myPHteam Member
I had the same problem with no insurance for a whole year after my diagnosis. Not a soul in the medical field I talked to knew anything about this disease. I applied for disability and was approved… read more